An infected wisdom tooth can be extremely painful and even pose a health risk.
Infections in these molars, also called third molars, usually arise due to the partial eruption of the tooth, which facilitates the accumulation of bacteria in the affected area.
Causes of an infected wisdom tooth
The most common causes of an infected wisdom tooth are usually related to infections in the gums or teeth. These can be caused by various factors, such as cavities, dental abscesses, food residue in the gums, as well as sores or canker sores.
Here are some of the common causes of infected teeth:
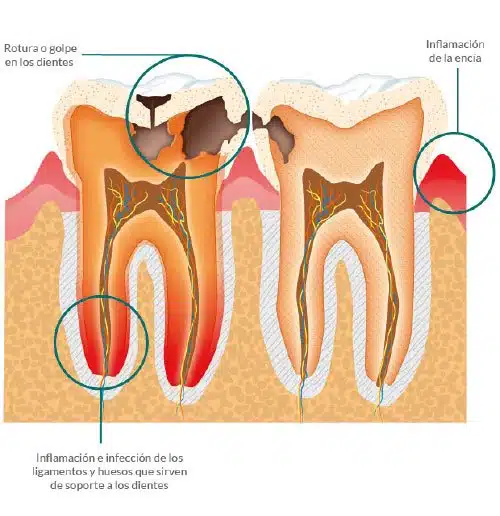
Dental Cavities: Cavities are a common reason behind dental infections. When harmful bacteria attack tooth enamel and penetrate the dental pulp (the innermost part that contains nerves and blood vessels), an infection can result. If left untreated, cavities can facilitate bacterial spread and result in pulp infection.
Dental Trauma: A blow or injury to a tooth, such as a fracture or crack, can open a door for bacteria to enter the inside of the tooth, causing an infection.
Dental Abscess: This is an accumulation of pus in the tooth or surrounding tissues. It may be the result of an untreated bacterial infection in the dental pulp or in the gums and bone around the teeth.
Gingivitis or Periodontitis: Infections in the gums (gingivitis) or in more severe cases of gum disease (periodontitis) can contribute to infection of the teeth, allowing bacteria to reach the area around the tooth root.
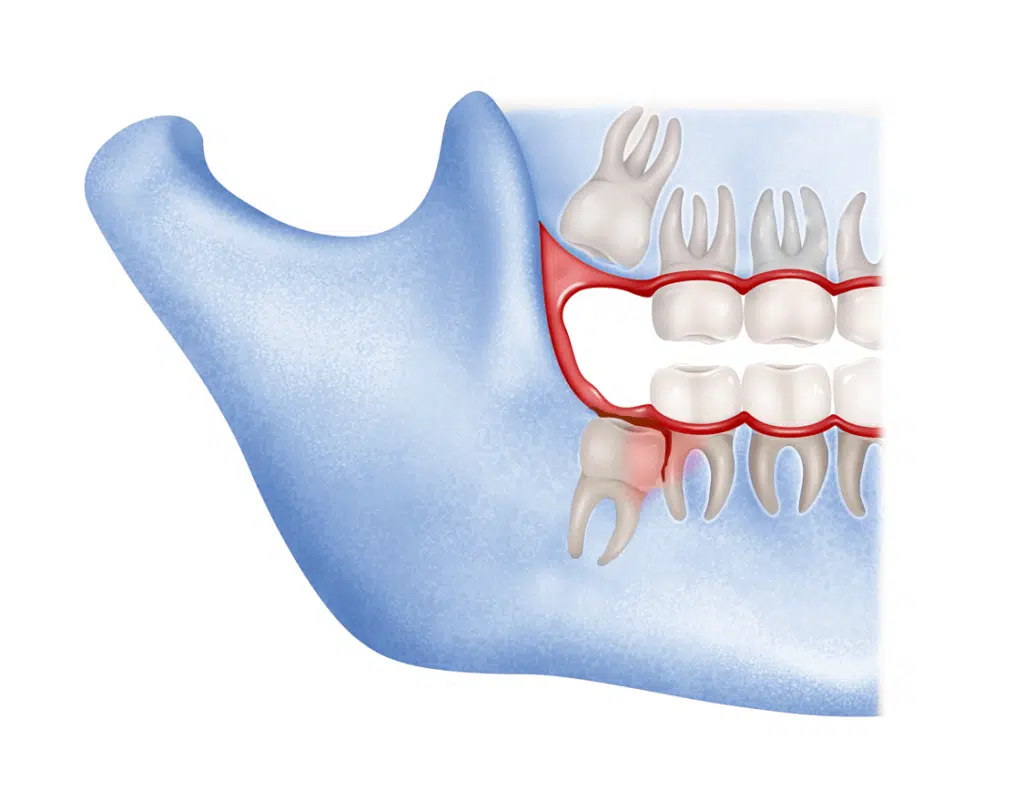
Impacted Teeth: Impacted teeth, such as third molars (wisdom teeth), often have difficulty erupting properly, which can create pockets or folds of tissue where bacteria can multiply and cause infections.
Systemic Diseases: Some medical conditions, such as diabetes, can increase the risk of dental infections by affecting immune system function.
Poor Oral Hygiene Habits: Lack of proper oral hygiene, such as not brushing or flossing regularly, can allow bacteria to build up in the mouth, increasing the risk of infections.
Genetic Factors: Some people may have a greater genetic predisposition to developing cavities or gum disease, which increases their risk of tooth infections.
Characteristic symptoms of infected teeth
Infected molars, usually caused by a bacterial infection within the tooth or adjacent tissues, can be painful and potentially dangerous if not treated properly. The characteristic symptoms of infected teeth can vary in intensity, but usually include the following:
Dental Pain: Pain is one of the most obvious symptoms of an infected tooth. It can manifest itself in a stabbing, pulsating or constant manner, and tends to increase over time. This pain may radiate to the jaw, ear, or neck.
Dental Sensitivity: The infected tooth can become extremely sensitive to heat, cold or pressure. Consuming hot or cold foods or drinks can cause intense discomfort.
Swelling: The infection can cause swelling in the area of the infected tooth, as well as in the cheek or surrounding tissue.
Bad Taste in Mouth: Some people may experience an unpleasant taste or bad breath due to the buildup of bacteria in the infected tooth.
Difficulty Chewing: Inflammation and pain can make it difficult to chew and use the affected side of the mouth.
Swollen Lymph Nodes: Sometimes, a tooth infection can lead to swollen lymph nodes in the neck.
Fever: In cases of severe infections, fever and general malaise may occur due to the immune system’s response to fighting the infection.
Abscesses: In more severe cases, the infection can spread and form a dental abscess, which consists of a collection of pus. This can cause significant swelling, severe pain, and the appearance of a pus-filled bump on the gum.
Infection of wisdom teeth or wisdom teeth
In such situations, the onset of the infection can even cause pain in the ears and/or throat, which can lead to confusion in the diagnosis. For this reason, it is crucial to see a specialist if you experience tooth pain, redness or inflammation. Getting an x-ray can help determine whether the problem lies with your wisdom teeth or not.
If the diagnosis of wisdom tooth infection is confirmed, it will be necessary to evaluate the severity of the infection and the condition of the tooth to decide if treatment should be followed to preserve it or if it is more appropriate to extract it.
In any case, it is essential to treat the infection in a timely manner to prevent the possible formation of abscesses that could complicate the situation and lead to the appearance of fever.
How and why does an infection occur in wisdom teeth?
Infection of wisdom teeth occurs when only a part of them emerges from the gum and the other remains trapped inside, forming a pocket in the gum that eventually becomes infected.
During feeding, food can become trapped in this bag due to the difficulty in performing proper hygiene in this hard-to-reach area. This can lead to the accumulation of bacteria, which in turn causes inflammation and eventually the appearance of an infection, dental abscess or phlegmon.
If it is not possible to remove the wisdom tooth immediately, the infection should be treated initially with antibiotics before proceeding with extraction.
In cases of more severe wisdom tooth infections, the inflammation can spread to the lymph nodes, which can cause difficulties swallowing, speaking or eating, a phenomenon known as pericoronitis.
Spread of wisdom teeth infection
If there is an infection in the molars, there is a risk that it will spread, which can cause serious complications such as involvement of the malar bone and surrounding soft tissues.
Possible routes of spread of wisdom teeth infection:
Local Spread: Dental infection in a wisdom tooth can spread to surrounding tissues, which can trigger a series of local complications, including the formation of a dental abscess. This abscess involves a buildup of pus in the infected area, which can cause swelling and severe pain in the jaw and cheek.
Infection of Adjacent Tissues: The infection can spread to nearby tissues, such as the gums, adjacent teeth, and jaw bones. This can lead to a more extensive infectious process that can be more complicated to treat.
Temporomandibular Joint Infection (TMJ): In severe cases, the infection can reach the temporomandibular joints, located in the jaw and responsible for mouth movement. An infection in these joints can cause pain and difficulty opening and closing your mouth.
Throat or Pharynx Infection: The spread of infection from the wisdom teeth to the throat or pharynx can result in a sore throat and difficulty swallowing.
Systemic Infection: In extremely rare and severe cases, wisdom teeth infection can spread through the blood, known as bacteremia. This can have serious implications for overall health, as bacteria can travel to other parts of the body, such as the heart or lungs, and cause life-threatening systemic infections.
What to Do if You Have an Infected Wisdom Tooth?
It is essential to seek immediate dental care. A dentist or maxillofacial surgeon will be able to diagnose the infection and determine the best course of action.
-Avoid self-medicating, as this can worsen the situation. Don’t try to drain a tooth abscess on your own.
-The dentist may prescribe antibiotics to control the infection. It is crucial to take them according to the specialist’s instructions.
-In many cases, dental treatment is necessary to eliminate the source of the infection. This may include a root canal (root canal treatment) or wisdom tooth removal.
-The dentist or oral surgeon may prescribe painkillers to relieve pain while the infection is treated.
-Follow your dentist’s instructions for home care, which may include saltwater rinses and maintaining good oral hygiene.
The correct treatment
for an infected wisdom tooth
The approach to treating an infected wisdom tooth usually focuses on clearing the infection, relieving pain, and preventing further complications. The choice of treatment will depend on the severity of the infection, the position of the wisdom tooth, and the patient’s general health. Below are treatment options for an infected wisdom tooth:
1. Antibiotics: In certain cases, the dentist or oral surgeon may prescribe antibiotics to control the infection. These medications are used to reduce inflammation and prevent the spread of infection to other areas. It is essential to follow your dental professional’s instructions exactly when taking antibiotics.
2. Dental Procedures:
– Endodontics (Root Canal Treatment): If the infection has reached the inside of the tooth (pulp), it may be necessary to perform a root canal to eliminate the infection and preserve the tooth. During this procedure, the infected pulp is removed, the tooth is cleaned, and sealed.
– Tooth Extraction: In many cases, especially if the wisdom tooth is impacted or non-functional, tooth extraction may be recommended followed by the possible placement of dental implants. Removal eliminates the source of the infection and prevents future problems. This procedure is performed under local anesthesia, and it is crucial to follow aftercare instructions.
3. Analgesia: To relieve the pain associated with an infected wisdom tooth, your dental health professional may prescribe pain relievers. Medical instructions should be followed and reported if pain persists or worsens.
4. Home Care: After treatment, it is important to follow the dentist’s instructions for home care. This may include saltwater rinses to keep the area clean and prevent bacteria buildup.
5. Follow-up: It is essential to schedule a follow-up appointment with the dentist or oral surgeon to ensure that the infection has resolved and that the extraction wound (if performed) is healing properly.